The principles of Patient Blood Management apply to all patients who may need transfusion.
In elective surgery the principles of PBM have been described as the so called '3 pillars' namely:
- Optimizing the patient's own blood (e.g. pre-operative optimization of haemoglobin and haemostasis)
- Minimising surgical blood loss
- Optimizing the patient's physiological reserve in relation to anaemia (including use of restrictive transfusion triggers)
However the key principles of PBM apply not just to surgery but to all patients who may need a blood transfusion (medical, obstetric, paediatrics), and to both elective and emergency clinical settings.
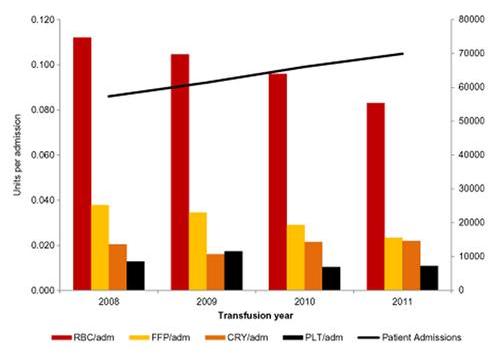
The overall use of red cells is decreasing in many countries but large audits still show much inappropriate use. Greater scrutiny is also needed in relation to appropriate use of platelet and plasma transfusion.
Accordingly, PBM covers all aspects of decision-making in transfusion therapy, including patient evaluation and clinical management with use of appropriate indications and triggers, minimization of blood loss and optimization of the patient's own red cell mass. By reducing the need for allogeneic blood transfusions and minimising risks and unnecessary work, PBM can also reduce health-care costs.
References
- Patient blood management. Goodnough LT & Shander A.Anesthesiology 2012; 116:1367-76.
- Transfusing blood safely and appropriately. Murphy MF et al.BMJ 2013;347 :f4303
- Restrictive blood transfusion practices are associated with improved patient outcomes. Goodnough LT et al.Transfusion 2014; 54: 2753–2759.
- Increased hospital costs associated with red blood cell transfusion. Trentino KM et al.Transfusion 2015; 55: 1082–1089.
- A pragmatic approach to embedding patient blood management in a tertiary hospital. Leahy MF et al.Transfusion 2014;54: 1133-45.
- Improving red cell transfusion in the elective surgical setting: an improvement collaborative with evaluation. Harrison BT et al.Vox Sanguinis 2015; 108: 393–402.
The authors